So, your doctor just told you that you have arthritis in one of your knees or even both knees…
The doctor also just told you that you need to run less if you want to be able to walk in 5 years…
“Rather take up swimming or cycling” – they say…as you look at them with disbelief in your eyes and a big lump in your throat.
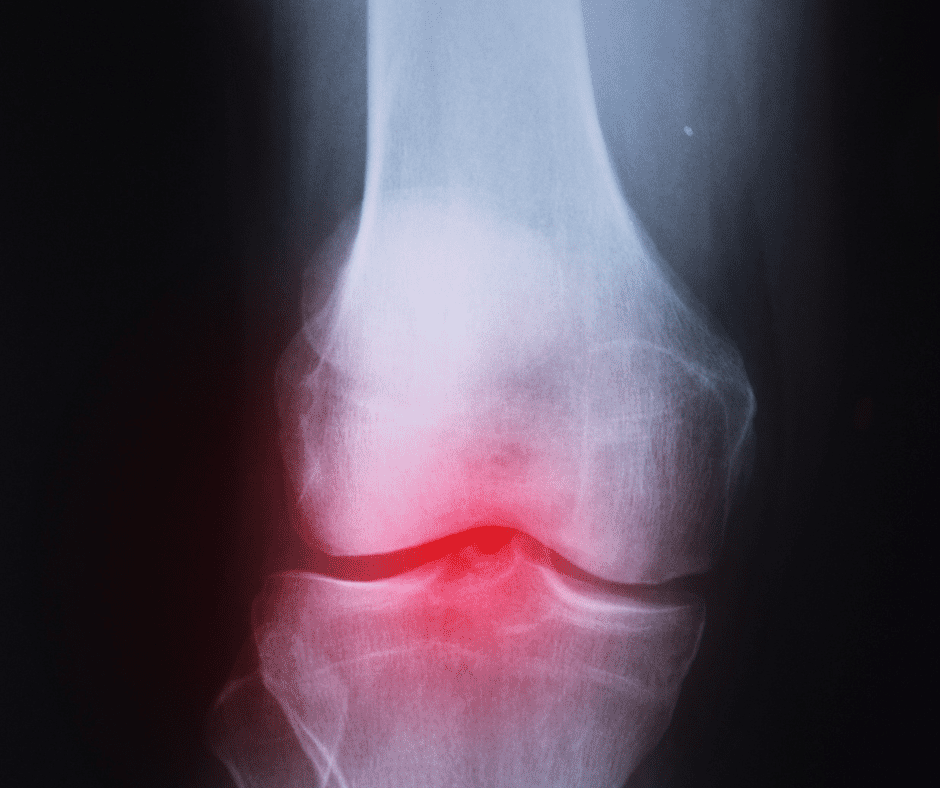
Arthritis in the knee is a degenerative and progressive, often painful disease that usually worsens with age.
You’ve got a half marathon planned in 6 months and are determined to continue running and doing what you love!
Is it possible to do just that? Let’s find out…
The Different Types Of Arthritis In The Knees
6 types of arthritis can affect the knee:
- Osteoarthritis
- Psoriatic Arthritis
- Gout
- Rheumatoid Arthritis
- Reactive Arthritis
- Pseudogout: Calcium Pyrophosphate Deposition (CPPD)
Osteoarthritis is the most common type found in one or both knees. According to a study, 3.5% of recreational runners have either knee or hip osteoarthritis compared to 10.2% of non-runners.
Osteoarthritis In The Knee
Osteoarthritis occurs when the protective cartilage that cushions the ends of the bones wears down over time.
Given the nature of the knee joint with its high use and frequent stress passing through it, it is often the site of conditions such as Osteo Arthritis.
Traditionally it was thought that the cartilage was the only tissue involved but the latest evidence indicates that OA is a multifactorial condition with various contributing causes including trauma, mechanical forces, metabolic changes, and inflammation.
Psoriatic Arthritis In The Knee
Psoriasis is a skin condition that causes skin cells to build up and form patches of itchy, dry skin called plaques.

If a person with psoriasis develops psoriatic arthritis as well, it may cause one or more joints, such as the knee, to become stiff, inflamed, and painful.
Gout In The Knee
Gout is a painful form of inflammatory arthritis that usually affects the big toe but can develop in any joint, including one or both of the knees.
Gout in the knee can be hot, red, swollen, and extremely painful to touch or move.
Rheumatoid Arthritis In The Knee
Rheumatoid Arthritis is an auto-immune condition, meaning that the immune system, which is your body’s natural self-defense system, gets confused and starts to attack your body’s healthy tissues.
It does this by causing inflammation in your joints.
Reactive Arthritis In The Knee
Reactive arthritis is a rare form of arthritis caused by bacterial infections.
This type of arthritis is often resolved on its own but can be prolonged.
Pseudogout: CPPD In The Knee
This is a form of arthritis characterized by sudden, painful swelling in one or more of your joints but commonly affects the knee.
Also called calcium pyrophosphate deposition disease or CPPD, and is considered quite similar to Gout although the type of crystal differs for each condition.
Causes Of Knee Arthritis
Firstly, let’s have a quick look at the bones of the knee…
Three bones come together to form your knee joint:
- Thighbone (femur).
- Shinbone (tibia).
- Kneecap (patella).
Cartilage (lubricated by the synovial membrane) covers the ends of each bone. It’s a cushion between the bones that keeps them from rubbing together.
What Causes Knee Arthritis?
Each type of arthritis in the knee has different causes… but in summary…
Experts have identified some genes that might cause arthritis of the knee.
Severe injury or repeated injury and overuse can also lead to knee osteoarthritis.
You could have a gene linked to arthritis without knowing it and a virus or injury could trigger it.
Though the exact cause of each is unknown, some risk factors increase the possibility of arthritis of the knee.

Risk Factors Of Osteoarthritis Include:
- Age
- Bone anomalies
- Gout, which might lead to osteoarthritis
- Injuries
- Stress
- Weight, extra weight puts more pressure on your knees
Signs/ Symptoms Of Arthritis In The Knee
- Creaking, grinding, or snapping noises from your knee.
- Pain increases when you are active, but gets a little better with rest.
- Swelling
- The feeling of warmth in the joint
- Stiffness in the knee, especially in the morning or when you have been sitting for a while.
- decrease in mobility of the knee.
- Joint pain that changes (gets better or worse) depending on the weather.
- Skin redness.
- Your knee locks or sticks when it’s trying to move.
Running With Knee Arthritis
According to the latest science, you can run with arthritis, and contrary to popular belief, running is not bad for your joints. Studies indicate that running helps ease arthritis pain and stiffness.
Let’s have a look at a study conducted by the Osteoarthritis initiative. The researchers had a look at the different levels of arthritis in a group of people as well as their pain levels.
They then took a look at the same group of people four years later and it turns out that those who continued to run had no increase in their symptoms as shown on x-rays and what is even more noteworthy is that they had less pain than they did four years ago.
It is possible that exercise, including running, can improve your symptoms and joint mobility whereas lack of activity could contribute to stiff joints and no improvement in pain.
It turns out that one of your body’s fantastic shock absorbers – cartilage, enjoys the cyclical loading associated with running.
Running with arthritis in your knees means there are a few extra considerations to take care of that will go a long way in reducing your risk of injury or aggravating your symptoms.
These are…
- Following a well-structured, scientific running training program.
- Correct running biomechanics, which you can improve with strength training, or in extreme cases – gait retraining.
- Avoid shuffling while you run. (Running biomechanics)
- Listening to your body, allowing adequate recovery time, and knowing when it’s time to slow down.
- Strengthening the musculoskeletal structures around your knees so that the load from running is better tolerated.
Osteoarthritis & Strength Training
A lot of people have this perception of…well… “squats are bad for my knees.”
Some scientific papers have come out lately that show over and over again, that resting full time and avoiding anything is worse for your knees… it makes the pain worse!
The addition of strength training and graded exercise has now been shown that it’s safe, and helps the pain overall. However, appropriate strength exercises should be prescribed by an exercise professional tailored to your individual ability and presentation of arthritis.
So, we must add in some aspects of strength, it’s not going to make it worse. Obviously… when done correctly.
It’s about the type of strength training that you’re doing and not saying just jump into plyometrics or anything, I’m talking about a safe and graded approach to exercise.
The same applies to running, if you have osteoarthritis and you decide you want to start running, you’re not going to go and run a marathon on your first weekend, you’ve got to build up slowly.
Here at Coach Parry, we’re massive advocates of strength training. We’ve put together this free strength training plan for runners that you can do once a week, at home and with no expensive equipment needed. You can access it by clicking here.
It is key to introduce strength training progressively.
A lot of papers have come out explaining high-value care vs low-value care.
Low-value care we have known about for years includes symptomatic relief like physio treatments and taking ibuprofen, or opioids to numb pain.
High-value care is adding strength training, adding lifestyle changes like weight loss, and doing the right sort of exercises that you need.
The message is that when there is pain that does not always equal damage and pain shouldn’t be ignored, we can make that joint stronger.
In the Coach Parry live strength classes, we often have people who have got osteoarthritis in their wrist joints as an example as well as arthritis in their knees and what we do is we actually modify the class for them and avoid exercises completely that we know would push them past their limits.



Comments are closed.